Alternative names for primary hyperaldosteronism
Conn’s syndrome; Conn syndrome; primary aldosteronism; hyperaldosteronism
What is aldosterone and why is it important?
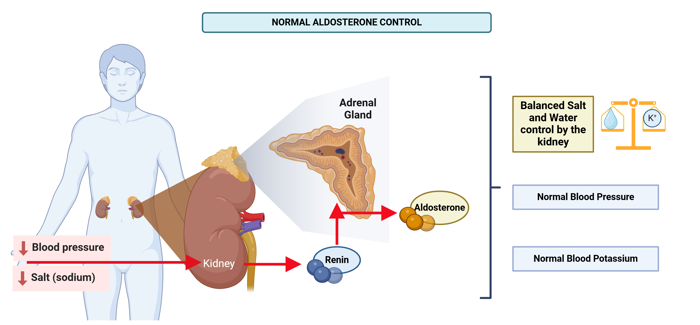
Figure 1: When blood pressure is low or there is not enough salt in the body, the kidney makes more renin. This signals the adrenal glands to release more aldosterone. Aldosterone helps the kidney keep the right balance of salt and water, which helps bring blood pressure and potassium levels back to normal. Image made using Biorender.
Aldosterone is a hormone made by the adrenal glands. The body has two adrenal glands, one each sitting on top of each kidney. Aldosterone helps keep the right balance of salt and water in the body by signalling the kidneys to hold on to some salt and water or release it into the urine. Aldosterone also stimulates the loss of potassium in the urine.
Renin is produced by the kidneys when the body is low on salt. It sends a message to the adrenal glands to make more aldosterone. This extra aldosterone helps the body save salt and water. Once the balance is restored, renin and aldosterone levels return to normal.
This is an example of a feedback system — like a thermostat that keeps the body’s salt balance.
What happens in primary hyperaldosteronism?
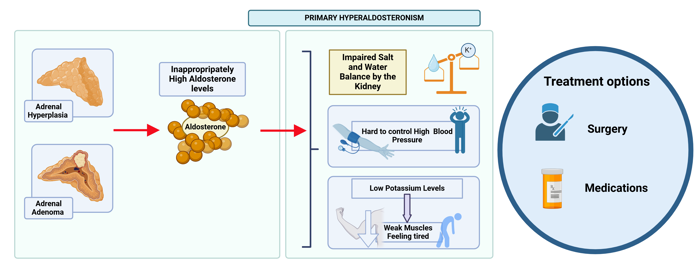
Figure 2: In Primary Hyperaldosteronism, the adrenal glands produce too much aldosterone due to hyperplasia (overgrowth) or an adenoma (benign tumour). This disrupts salt and water balance, leading to high blood pressure and low potassium, which can cause weak muscles and tiredness. Treatments include surgery and medication. Made using Biorender.
Hyperaldosteronism refers to any state where there is excessive or inappropriately high levels of aldosterone in the bloodstream. In primary hyperaldosteronism, the adrenal glands make too much aldosterone even when the body doesn’t need it.
This causes the body to hold on to extra salt, which leads to:
- High blood pressure (hypertension)
- Losing potassium (an important mineral) in the urine, which leads to low potassium levels in the blood. This can result in symptoms such as weakness, tiredness, or muscle cramps but often patients may be asymptomatic.
Primary hyperaldosteronism is different from secondary hyperaldosteronism. Secondary hyperaldosteronism occurs when the kidneys produce too much renin, and therefore also aldosterone. It can happen due to other illnesses like heart, kidney or liver disease.
What causes primary hyperaldosteronism?
There are a few reasons why the adrenal glands might produce too much aldosterone:
- Adrenal hyperplasia: Overgrowth of one or both adrenal glands (called hyperplasia). This extra growth causes too much aldosterone to be made.
- Adrenal adenoma: A small, non-cancerous lump (also known as tumour) in one adrenal gland can make extra aldosterone.
- Adrenal carcinoma: In very rare cases, a large cancerous lump or tumour in the adrenal gland may produce aldosterone.
- Rarely, people inherit conditions that cause a similar picture to primary hyperaldosteronism to a genetic mutation (change in DNA).
In all these cases, the normal feedback system controlling aldosterone production is disrupted, leading to continued hormone production even when it’s not needed.
What are the signs and symptoms of primary hyperaldosteronism?
Many people with primary hyperaldosteronism don’t feel sick or notice any obvious symptoms. This condition is often discovered during routine checks for high blood pressure, especially when the condition doesn’t improve even after taking multiple blood pressure medications. Patients with primary hyperaldosteronism may be diagnosed very late as the symptoms can be subtle.
Symptoms may include:
- High blood pressure is the most common symptom: that is hard to control (i.e. requires many medications) or in a young patient.
- Low potassium levels, which may cause:
- Muscle cramps.
- Weakness or feeling very tired.
- Excessive thirst or frequent urination.
How common is primary hyperaldosteronism?
Primary hyperaldosteronism is now believed to be more common than previously thought. It may affect roughly one in ten people with high blood pressure. Among those with resistant high blood pressure, which is difficult to control with medication, it could be as high as one in four.
The condition is often diagnosed in adults between their 30s and 40s, with certain types, like adrenal adenomas, being more frequently found in women.
While exact numbers might vary over time, awareness and improved testing are making it easier to recognise this condition.
Is primary hyperaldosteronism inherited?
The most common causes of hyperaldosteronism (adrenal hyperplasia and benign adrenal tumours) are not usually inherited. However, rare types exist that can run in families.
What are the long-term effects of primary hyperaldosteronism?
If untreated, the high blood pressure caused by this condition can increase the risk of:
- Heart disease or heart attacks
- Strokes
- Damage to blood vessels, kidneys, or eyesight
With appropriate treatment, these risks are greatly reduced. Patients who need long-term medication will require regular doctor check-ups to monitor their blood pressure, potassium levels, and overall health.
How is primary hyperaldosteronism diagnosed?
Doctors might suspect primary hyperaldosteronism in patients with:
- High blood pressure that doesn’t improve with medication or requires multiple medications.
- Low potassium levels in the blood.
Endocrinologists, doctors who specialise in hormone-related conditions, usually manage the diagnosis and treatment. Common tests to help make a diagnosis include:
- Blood tests: Both renin and aldosterone can be measured in the bloodstream. A high aldosterone and low renin would raise the suspicion of primary hyperaldosteronism. For this reason, doctors will first check aldosterone and renin levels in the bloodstream. These tests are usually done in the morning while sitting or lying down.
- Salt challenge test: A ‘salt challenge’ test may be carried out. In this test, aldosterone levels are checked after giving a salt solution (saline) drip directly into the bloodstream. In a healthy person, aldosterone levels should fall after the infusion of saline. This does not happen in primary hyperaldosteronism.
- Adrenal gland scan: To find a cause (e.g. diffuse adrenal swelling or adenoma), doctors may organise a CT/MRI scan of the adrenal glands to look for a benign tumour or gland swelling.
- Special vein cannulation test (Adrenal Venous Sampling): If imaging isn’t clear, doctors may measure aldosterone levels directly from the veins draining the adrenal glands using a tiny tube to collect the blood under local anaesthetic. Newer nuclear medicine imaging techniques are also being developed to enable doctors to localise small adrenal abnormalities that were not previously visible as potential targets for surgical removal.
In rare cases, genetic testing may be done if inherited forms are suspected (for example if glucocorticoid-suppressible hyperaldosteronism is suspected).
How is primary hyperaldosteronism treated?
The treatment of primary hyperaldosteronism depends on the underlying cause and the patient’s overall health.
If a benign tumour (adenoma) is the cause, this can be removed with keyhole surgery (laparoscopic adrenalectomy) if the patient is fit enough for surgery. This is done by an expert adrenal surgeon (usually an endocrine surgeon) and is usually very safe with few complications.
Surgery often improves potassium levels and blood pressure, and patients may no longer need blood pressure medication after surgery.
Surgery is usually not recommended if the cause is swelling of both adrenal glands (adrenal hyperplasia) because if just one adrenal is removed, the other enlarged adrenal will still produce too much aldosterone and this will have little impact on future blood pressure. Also, the adrenal glands produce other hormones that are very important to normal body functions, such as cortisol, therefore it is not recommended for both adrenals to be removed. In these situations, or if a surgery is not an option due to the patient’s overall health, medications like spironolactone or eplerenone are used.
These medications block the effects of aldosterone and can also lower blood pressure and improve potassium levels.
Are there any side-effects to the treatment?
Medications:
- May cause high potassium levels (hyperkalaemia) or low salt levels (hyponatraemia) in the blood as it blocks the action of aldosterone.
- Spironolactone specifically may affect other hormones, causing:
- Irregular periods in women.
- Breast swelling and tenderness or impotence in men, as it blocks the action of testosterone.
- During pregnancy, spironolactone is not recommended due to potential harm to the developing baby.

