Alternative names for toxic thyroid nodule?
What is a toxic thyroid nodule?
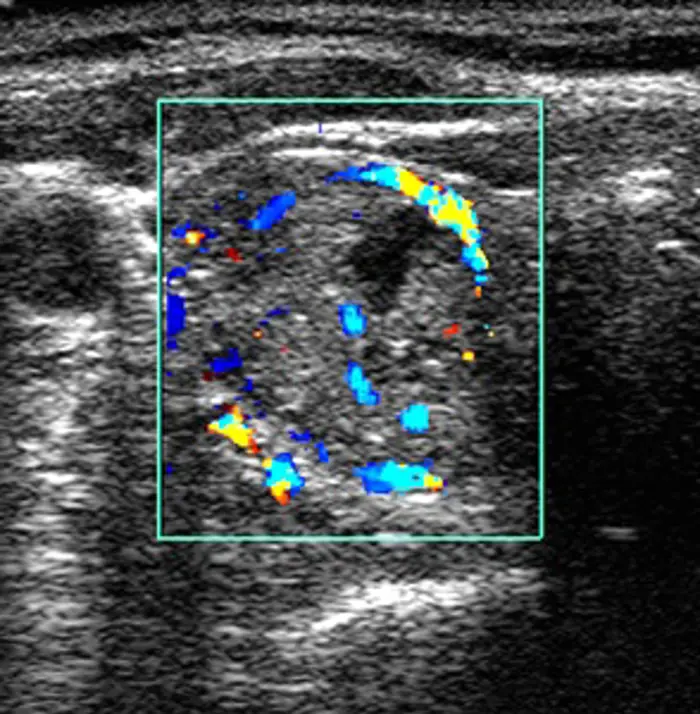
Ultrasound scan in transverse section of the thyroid gland of a 73-year-old female patient, showing a hot nodule (increased activity) in one thyroid lobe corresponding to a toxic adenoma.
A toxic thyroid nodule is a cause of hyperthyroidism (an overactive thyroid gland), which is a cause of thyrotoxicosis (having an excess amount of thyroid hormones). This occurs when a single nodule (or lump) grows in the thyroid gland and produces excess thyroid hormones. Toxic nodules are usually benign (ie non-cancerous). If the increased hormone production is coming from a single nodule in the gland, this is called a ‘toxic nodule’. If the thyroid gland becomes enlarged, for example due to the presence of nodules, this is called a ‘goitre’. If there are many nodules causing hyperthyroidism, this is referred to as a ‘toxic multinodular goitre’.
What are the signs and symptoms of a toxic thyroid nodule?
The symptoms of a toxic thyroid nodule are a result of the high levels of thyroid hormones in the blood, increasing the rate at which the body is working.
This results in hyperthyroidism and symptoms of thyrotoxicosis including:
- weight loss
- diarrhoea
- increased appetite
- flushing
- irritability
- tiredness
- palpitations (increased heart rate which can be felt by the patient)
- poor sleep
- increased sweating
- a tremor
- heat intolerance (feeling excessively hot even though others may find it cold).
How common is a toxic thyroid nodule?
Thyroid disorders are much more common in women than in men. Figures from the USA state that the incidence of toxic thyroid nodules accounts for 3–5% of patients with hyperthyroidism. Toxic nodules are more common in elderly people, particularly in areas of iodine deficiency.
Are toxic thyroid nodules inherited?
Currently, toxic nodules are not thought to be inherited.
How is a toxic thyroid nodule diagnosed?
Diagnosis is very similar to that of hyperthyroidism. A full medical history is taken, and a blood test is carried out to measure thyroid hormone levels. The thyroid gland will be examined for presence of nodule(s). Thyroid antibodies are used to assist in the diagnosis (in Graves’ disease, antibodies against the TSH-receptor are typically present, but would not be present in a nodular goitre).
An ultrasound scan of the neck is usually carried out to assess the thyroid nodule, and a sample of cells from the thyroid nodule may be taken for analysis. This involves inserting a small thin needle into the nodule to collect a sample, which can then be analysed in the laboratory. This procedure is not painful, but can feel uncomfortable. It is not recommended to take a sample when the patient is in a hyperthyroid state.
In a small number of cases, if the goitre is large, other tests such as lung function tests may be carried out to assess whether breathing is affected. Rarely, a computerised tomography (CT) scan may also be performed to obtain a more detailed image of the gland.
A thyroid iodine uptake scan may also be performed. This is a test to measure how much iodine is taken up by the thyroid gland and gives an indication of whether the thyroid gland is under or overactive. A toxic nodule can have increased uptake of iodine within the nodule which is referred to as a ‘hot nodule’, with the rest of the gland suppressed. All these investigations can be performed in the outpatient department.
How is a patient with a toxic thyroid nodule treated?
There are three main treatment options:
- Radioiodine is the most effective treatment to cure a toxic nodule. It involves the patient taking either a capsule or liquid containing radioactive This can be carried out in the outpatient department. Iodine is used mostly by the thyroid gland so that all the radioiodineis concentrated in the gland and causes a gradual destruction of it. In the case of a hot nodule, the aim is for the nodule to take up the radioiodine and be destroyed whilst the rest of the gland is spared. The iodine does not affect any other part of the body and is a safe treatment. However, there are temporary restrictions such as avoiding close contact with children and pregnant women in the first few weeks following treatment.
- Surgery may be carried out to remove the toxic nodule, which will treat the hyperthyroidism. If the nodule is large, surgery will relieve the compressive symptoms of the enlarged thyroid such as breathing and swallowing difficulties. If a total thyroidectomyis carried out (to remove the whole thyroid gland), thyroid hormone replacement will need to be taken for life. Surgery is usually very effective, but a small number of patients can develop recurrence of the nodules.
- Medication: anti-thyroid drugs such as carbimazole are used to control the overactive thyroid symptoms, and it may need to be taken long-term. Carbimazole, which is taken as tablets, is mainly used either before surgery to control symptoms or in patients where other treatment options are not possible.
Are there any side-effects to the treatment?
Radioiodine: A minority of patients (around 1%) experience a sore feeling or discomfort in the front of the neck following radioiodine treatment. The radioiodine can also cause the thyroid gland to become underactive in some cases. The patient would then need to take tablets to replace the thyroid hormone. It is also important for patients having radioiodine treatment to stay away from children and pregnant women for three weeks to avoid exposing them to radiation. Patients should speak to their doctor about pregnancy as it should be avoided for up to six months after radioiodine treatment. Patients should discuss any concerns with their doctor. More information on the practicalities of radioiodine treatment can be obtained from the hospital’s Medical Physics department where the treatment will take place.
Surgery: There are general risks of surgery and anaesthesia, which should be reviewed by the surgeon or anaesthetist. Rare side-effects include damage to the recurrent laryngeal nerve, which runs close to the thyroid gland in the neck, and can affect or alter a patient’s voice if damaged (causing a hoarse voice). The parathyroid glands are attached to the thyroid gland and can be temporarily or permanently injured during the surgery causing hypoparathyroidism. This would require the patient to take calcium and vitamin D supplements for life. However, in some cases one of the parathyroid glands can be preserved in the body and normal parathyroid function is restored. These should be discussed with the patient before surgery. If the whole thyroid gland is removed, thyroid hormone replacement tablets (thyroxine) will need to be taken for life.
Medication: Taking carbimazole tablets can cause side-effects such as reducing the number of white blood cells in the body; however, this is very rare. Patients who develop a sore throat or raised temperature whilst taking carbimazole should see their doctor as soon as possible.
What are the longer-term implications of a toxic thyroid nodule?
The long-term implications of a toxic thyroid nodule depend on the treatment option used. Patients taking carbimazole tablets will likely need to take them daily for life. Blood tests should be carried out regularly to monitor thyroid hormone levels and to adjust the dose of carbimazole accordingly. Most patients are able to find a medication regimen that works for them and go on to live full, active lives.
If the increased thyroid hormones are not treated, besides feeling poorly and unwell, the patient is at risk of heart dysfunction or failure due to the increased heart rate and raised metabolic state. This irregular heart rate can result in strokes and dizziness. Long-standing toxic nodules can also affect the patient’s bones and cause osteoporosis, which results in weak bones that are more likely to fracture.
Rarely, if the nodule is very large, the patient may also develop symptoms due to the enlarged thyroid gland such as difficulty with breathing or swallowing (as the enlarged gland may press on the food or wind pipes, which are located nearby). If patients have any concerns about this condition, they should discuss them with their doctor.
Are there patient support groups for people with a toxic thyroid nodule?
British Thyroid Foundation may be able to provide advice and support to patients and their families dealing with toxic thyroid nodule.

