Alternative names for IVF
Together with other fertility treatments, IVF treatment can be referred to as assisted reproductive technology (ART).
What is IVF treatment?
A number of steps are required during IVF treatment, many of which simulate physiological processes in the natural menstrual cycle:
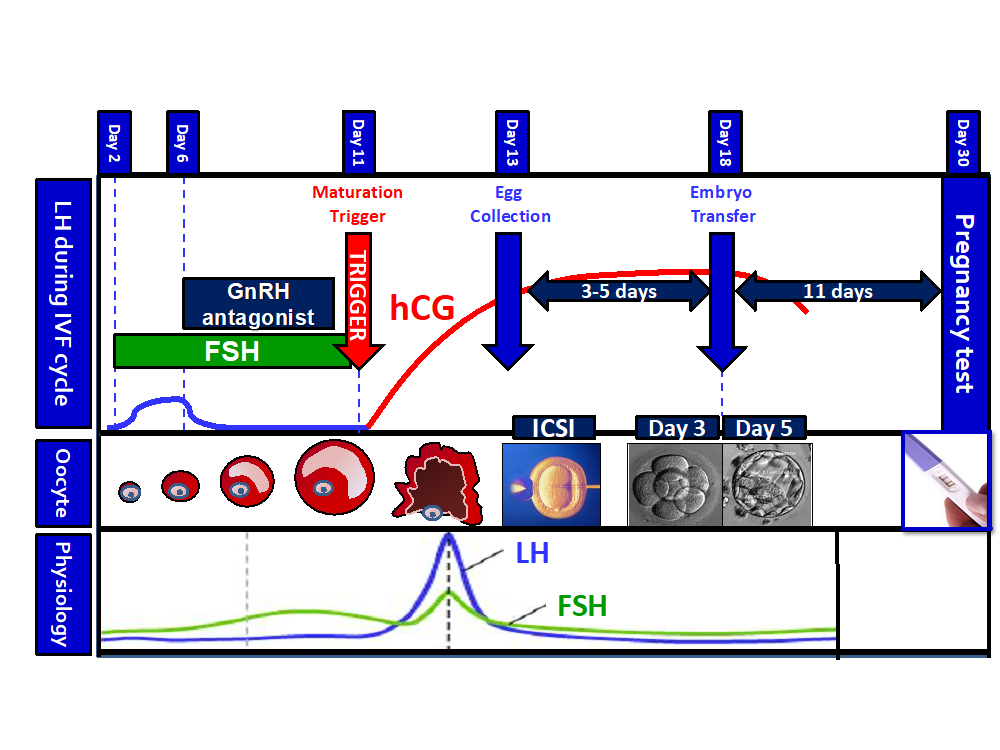
Visual representation of an IVF cycle
- Follicle growth: Whilst in the natural menstrual cycle, perhaps only 1 or 2 follicles will grow each month, in IVF treatment a large dose of synthetic follicle stimulating hormone (FSH) is used to induce the growth of multiple follicles in the ovary. This is termed either ‘superovulation’, ‘controlled ovarian stimulation’, or just ovarian stimulation.
- Prevent premature ovulation: In IVF, eggs are retrieved directly from the ovary, therefore it is important to prevent premature ovulation (release of the egg from the follicles in the ovary into the fallopian tubes) from occurring. Otherwise, there will be no egg remaining within the ovary to be collected during the surgical egg retrieval. Ovulation is caused by a rise in luteinising hormone (LH) in the middle of the natural menstrual cycle. Thus, prevention of premature ovulation is achieved by using a medication that can prevent a premature rise in LH. Preferably, this is done by giving a GnRH antagonist (blocker of GnRH receptors in the pituitary gland), which prevents the subsequent rise in LH. This protocol is better for the risk of ‘Ovarian Hyperstimulation Syndrome’ (OHSS), a dangerous side-effect of IVF treatment. Alternatively, a GnRH agonist (stimulator) can be used. Although technically a stimulator of GnRH receptors, if a GnRH agonist is given at high doses persistently, they lead to suppression of the GnRH receptor and act similarly to a blocker. Thus, GnRH agonists can similarly be used to prevent a rise in LH levels.
- Maturation of eggs: Initially, LH is blocked as described above, to prevent premature ovulation and allow the follicles the time they need to reach the required size. Once the follicles reach this size, a medication is required to provide LH-like activity to ‘mature’ the eggs. ‘Maturation’ of the eggs refers to their gaining the capability to be fertilised by sperm. During the maturation process, the amount of DNA in the egg is halved such that the remaining half of the DNA can be provided by the sperm during fertilisation. An immature egg is referred to as ‘metaphase I’ and a mature egg as ‘metaphase II’. Only mature (metaphase II) eggs can be fertilised by sperm and immature eggs are difficult to retrieve from the ovary. In order to mature the eggs, a hormone is given usually 36-38 hours prior to collecting the eggs. The most commonly used hormone is human chorionic gonadotrophin (hCG), which can act on the receptors for LH and provide LH-like activity. Other hormone options that can be used to mature eggs include a GnRH agonist (stimulator), which stimulates the pituitary gland to secrete LH, which then in turn acts on the ovaries to mature the eggs.
- Surgical Retrieval of Eggs: The eggs are collected directly from the ovary via a small operation.
- Fertilisation: The eggs are then fertilised in the laboratory with sperm to form embryos. This can either be by mixing the eggs with the sperm and allowing fertilisation to occur spontaneously. Alternatively, a more technical form of fertilisation is needed, especially if there are issues with the quality or number of sperm. One such example is Intra-Cytoplasmic Sperm Injection (ICSI), which refers to selection of a single sperm and directly injecting it into a mature egg to achieve fertilisation.
- Embryo Selection: After 3-5 days, the best 1-2 embryos are selected for transfer back to the endometrium (womb). If more than one embryo is selected for transfer, this can result in a multiple pregnancy (twin or triplet), which is not healthy for the mother or the babies. Thus, increasingly, it is encouraged that only one embryo is transferred back to women with a good chance of pregnancy.
- Embryo transfer: The best embryo is transferred back to the endometrium via a small procedure at 3-5 days after the egg retrieval.
- Luteal Phase Support: Usually, most women are prescribed hormones to ensure that the womb is receptive to the embryo, which is called ‘luteal phase support’. Luteal phase support usually consists of progesterone supplementation, and sometimes also oestrogen supplementation.
- Pregnancy test: A pregnancy blood or urine test is carried out ~11 days after the embryo transfer procedure.
- Confirmation of clinical pregnancy: An ultrasound scan is then carried out 14 days later to confirm that the embryo is alive. Patients are usually discharged after this point to regular antenatal care.
Thus, an IVF cycle usually takes about 6 weeks and involves a number of steps with multiple visits to the hospital required.
What causes infertility?
Infertility is defined as an inability to conceive after 1 year of regular intercourse. This can be due to problems with sperm (termed ‘male factor’ infertility), or with female reproduction, and can often be with both. In females, common causes include a lack of ovulation (termed anovulatory infertility e.g. due to polycystic ovary syndrome, PCOS), a problem with the fallopian tubes (termed ‘tubal infertility’ e.g. pelvic inflammatory disease), or endometrial causes (problems with the lining of the womb e.g. fibroids).
What are the signs and symptoms of infertility?
Infertility is usually not associated with symptoms. Absent or irregular periods could suggest a lack of ovulation. Excess androgens causing excess hair growth or acne can also be a feature of PCOS which can cause lack of ovulation. Pelvic pain could indicate issues such as endometriosis.
How common is infertility?
One in six couples suffer with infertility and approximately 70,000 cycles are carried out for fertility treatment each year, with ~2% of babies born through IVF treatment. The latest figures in the UK can be found on the HFEA website.
How is infertility diagnosed?
The male partner will have a sperm test. The female partner may have their progesterone level tested in the middle of the luteal phase (e.g. 21st day of the menstrual cycle) to see if she is ovulating. She will also have an ultrasound scan to see how many follicles she has in the ovary called the ‘antral follicle count’; this can indicate how likely she is to respond to the hormones used during the IVF cycle and how likely she is to have a baby after her IVF cycle. A blood test for anti-Müllerian Hormone (AMH) can provide similar information. An ultrasound scan can also pick up other abnormalities, such as fibroids. A test is usually also carried out to check that the fallopian tubes are healthy and patent such as a Hystero-Salpingo-Gram (HSG) or Hysterosalpingo Contrast Sonography (HyCoSi).
How is infertility treated?
Fertility is treated depending on the identified cause, but if no cause is found, this is termed ‘unexplained infertility’. If a problem with ovulation is found, then medications to restore this can be trialed before IVF treatment. After other treatments have been trialed, IVF treatment can be trialled.
Are there any side-effects to the treatment?
The most severe side-effect is ovarian hyperstimulation syndrome (OHSS). This is most often caused by the use of human chorionic gonadotrophin (hCG) to induce maturation of eggs. Unfortunately, hCG has a long duration of action (> 1 week) and can result in overstimulation of the ovaries. This can lead to the release of dangerous chemicals from the ovary (e.g. vascular endothelial growth factor; VEGF) that make the blood vessels in the body leaky. This can cause leakage of fluid from the blood vessels to areas which normally don’t contain fluid, such as the lungs and the abdomen. Therefore, OHSS can be associated with swelling of the abdomen (termed ascites), shortness of breath due to fluid in the lungs (termed pleural effusion), abnormal kidney function (due to lack of fluid in the blood vessels in the kidney) and swelling of the ovaries which can then twist (termed ovarian torsion). Symptoms of OHSS can include feeling sick (nausea), vomiting, abdominal pain, abdominal swelling and breathing difficulties.
What are the longer-term implications of infertility?
Many couples suffering with infertility have significant rates of anxiety and depression, and unfortunately many relationships are broken by infertility.
Related websites
Human Fertilisation and Embryology Authority
Last reviewed: Feb 2021