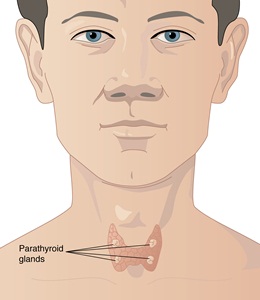
The parathyroid glands are located in the neck, just behind the butterfly-shaped thyroid gland
There are four parathyroid glands, situated in the front of the neck, and they are normally about the size of a grain of rice. The main action of parathyroid hormone is to keep blood calcium levels in a set range. It does this by regulating the amount of calcium passed out in the urine and increasing calcium release from bones.
Tertiary hyperparathyroidism usually happens after long-term secondary hyperparathyroidism when the parathyroid glands have been producing high levels of parathyroid hormone for such a long time that they become overgrown and permanently overactive. This leads to high blood calcium levels.
The most common cause of tertiary hyperparathyroidism is chronic kidney disease. It can continue even after a kidney transplant. High phosphate levels, low levels of active vitamin D and hypocalcaemia, all typical symptoms of kidney disease, cause long-term high parathyroid hormone and overgrowth of the parathyroid glands. Tertiary hyperparathyroidism can also occur in people who need to take phosphate treatment; for example, in a rare inherited disease called hypophosphataemic rickets. It often affects all four parathyroid glands, but sometimes just one or two glands.
The signs and symptoms are usually similar to primary hyperparathyroidism with a risk of reduced bone density (osteoporosis), muscle weakness, bone pain, constipation, abdominal pain, poor concentration or confusion. This is because of the high parathyroid hormone and high blood calcium caused by the condition.
It is rare, and mostly affects people with chronic kidney disease.
No.
Blood tests will show raised calcium and parathyroid hormone levels. Phosphate levels can be variable, dependent on kidney function.
The high blood calcium levels may be controlled with a drug called Cinacalcet. However, the definitive treatment is surgery, which involves partial or total removal of the parathyroid glands (parathyroidectomy). If there is total removal (all four glands are removed) a small piece of healthy parathyroid tissue can be implanted into the forearm to maintain parathyroid hormone levels, or patients can take vitamin D and calcium supplements lifelong.
If all four parathyroid glands are removed, this will result in no production of parathyroid hormone, and hypoparathyroidism may develop. This will need to be treated with activated forms of vitamin D and calcium supplements. The risks of parathyroidectomy are the same as for primary hyperparathyroidism.
Untreated tertiary hyperparathyroidism is associated with similar risks to those of primary hyperparathyroidism.
Parathyroid UK may be able to provide advice and support to patients and their families dealing with tertiary hyperparathyroidism.
Last reviewed: Feb 2018